Free article on Suspender Nickel dermatitis – prevention is the key
Review of: ‘ Suspender ’ Dermatitis and Nickel Sensitivity
Original article: D. Calnan and G. C. Wells. (1956). Suspender Dermatitis and Nickel Sensitivity. British Medical Journal, 1(4978), p. 1265-1268.
Reviewed by Brittanya Limone, BS, MA, MSIII, Loma Linda University.
- Historically, nickel allergy contact dermatitis was primarily associated with women working in industrial processes.
- Calnan and Wells use a case of suspender dermatitis, one of the most common causes of nickel allergic contact dermatitis c. 1956, to highlight the prevalence of this condition amongst women regardless of their employment.
- A dermatitis reaction is thought to occur after friction and sweat wear on nickel-containing products. These mediums gradually remove the nickel coatings and allow for nickel ion absorption across one’s skin.
- In addition to suspenders, other everyday nickel-containing products that may induce an allergic contact dermatitis include watches, bra clasps, and earrings.
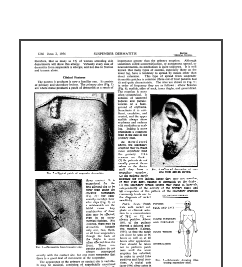
- Typically, the first reaction site occurs in direct contact with the metal, also known as the primary site. This region appears as excoriated, superficial papules or a confluent patch.
- Of note, pierced earrings were noted to cause earlobe dermatitis with crusts and exudates that might be mistaken for impetigo (infection).
- Eruptions at sites distant to the metal’s direct contact are secondary sites. These occur in a symmetric fashion on the eyelids, sides of the neck, inner thighs, and elbow flexures.
- Secondary reactions develop as papules or vesicles overlying an erythematous, edematous background with or without crusts and exudates.
- A secondary flare-up is a more important clinical feature for diagnosis and treatment.
- In terms of diagnosis, patients might not typically seek medical care until a secondary eruption. Therefore, recognition of these lesions, more commonly, leads to the diagnosis of nickel sensitivity.
- However, conditions with secondary flare-up reactions are more difficult to treat. Patients with a primary lesion respond quickly to therapy, but once a secondary eruption occurs, clearing the condition is difficult and recurrences are more common.
- Patch testing is used to confirm the diagnosis of nickel allergic contact dermatitis. However, waiting for the alleviation of an acute exacerbation is important as false positives from local reactions to patch testing may occur.
- Prevention is key to this condition’s treatment and reduces recurrences.
- The first step is the removal of all jewelry, metal clips or fasteners.
- If nickel-containing products must be worn, then they should be covered with a protective coating of fabric, plastic, or enamel.
- Alternatively, replacement products may be used such as items made of 100% plastic or nylon.