The Dermatitis Academy Story
It was 2004, Europe had instituted the European Union Nickel Directive limiting the allowable release of nickel from items that were in direct and prolonged contact with the skin and the sensitization (allergy) rates to nickel were plummeting. I became aware of this great need in the United States and decided to pursue training at NYU with Dr. David Cohen in contact dermatitis. That same year, at the University of Miami, we conceived the business model for an institute for contact dermatitis that would serve the growing needs of patients with contact dermatitis by offering the highest tier of comprehensive patch testing, serve the needs of trainees who could come to the center to learn in partnership with excellent patient care, and provide the most up-to-date evidence-based resources for education. This marked the inception of the Dermatitis Academy.
Over the next three years, we grew the contact dermatitis practice at the University of Miami serving contact dermatitis needs throughout South Florida with referrals from Mexico, central and south America. We trained dermatology residents and began a training program for Fellows and Affiliate Providers and laid the foundation for informational and interactive educational resources.
During this time I became actively (passionately) involved in a campaign for safer regulation of nickel in the US. In 2008, as a member of the Public Relations Committee of the American Contact Dermatitis Society, we presented a resolution to the American Academy of Dermatology (AAD) to issue a health advisory and document a need for an EU-like nickel directive in the United States. In response, the AAD developed a Nickel Workgroup, which formalized the resolution and ultimately the Council on Government Affairs and Health Policy and Practice approved and presented to the American Medical Association House of Delegates (AMAHOD). In June 2011, the AMA-HOD adopted the nickel resolution and sent a letter to the Consumer Patient Safety Commission (CPSC) regarding nickel:
“The AMA urges the CPSC to protect the public health by issuing safety standards that would limit the amount of nickel in consumer products with prolonged skin contact.” The Deputy Executive Director for Safety Operations at the CPSC responded, “The issue of nickel sensitization and consumer products is one that the CPSC and its staff have been aware of since the agency’s inception” (CPSC inception was in 1972)!
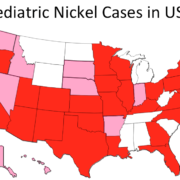
In February 2015, we formally launched the Dermatitis Academy in partnership with the Nickel Allergy Alliance to track the pediatric and adult cases of nickel in the US and bring awareness to this silent epidemic. We redrafted a nickel resolution and submitted it to the American Contact Dermatitis Society’s (ACDS) Health Policy Committee. In partnership with this committee, the American Academy of Pediatrics, the American Academy of Allergy Asthma and Immunology and the American College of Asthma Allergy and Immunology and the National Eczema Association the resolution was finalized and submitted to the AAD, which approved the resolution and formed a nickel workgroup to study the issue and develop a position statement. In August 2015, the AAD publicly issued a nickel position statement.
Twelve years later, I am still actively engaged in this public health campaign. In March 2016, the Dermatitis Academy launched the free website to expanded the outreach, to provide educational resources on the most prevalent allergens identified through evidence-based meta-analysis of the literature, webinars, and the Simple and Free™ guideline.
This month (May 2016), just two months since the launch of the public website, we have had over 31,000 visits to our site… We hope you find the Dermatitis Academy a useful education tool… please share.